Chemo No. 1
This week is 4 weeks post-op from my double mastectomy and recovery is going well. I’m working with a physical therapist to regain mobility and strength, stretches to do 3 times a day, and slowly working up to doing my normal daily activities again. The temporary expanders are slightly uncomfortable still… think tupperware in your chest, that’s the best way I can explain it.
Tuesday morning my lifting restrictions for my double mastectomy were over, it felt amazing to pick H up out of his crib in the morning! My port placement surgery was later that day, with new lifting restrictions. Having young children during cancer treatment adds an entire layer of challenges and heartache, with little ones being so dependent on their caregivers. I work from home with H with me most of the day and E at home in the afternoons, I was the person they depended on. To not be that main person for them right now breaks my heart, but I constantly remind myself that I need to take care of myself and accept help now so I can be that person again for them. I’m having to rewrite my role as ‘mommy’ right now, and some days are really hard - I get in a funk when I can’t ‘do it all’. It’s hard for us all when there lacks consistency with everything changing so often, but with help from the grandmas we try to keep E & H on their daily routines and show them love in every way possible.
The idea of a chest port completely grosses me out, but after my first treatment I am so grateful for my lovely port friend. My first infusion day was yesterday - my treatment plan is weekly Taxol (chemotheorapy) for 12 weeks, and Herceptin (targeted immunotherapy for being HER2+) every 3 weeks for a year. HER2 proteins are receptors that control how the cancer cells grow and divide, because of this HER2+ breast cancer can be aggressive. Herceptin is the key to targeting the HER2 proteins and telling my immune system to evict them, it’s my lifeline, my insurance to make sure this cancer does not return. A once terrible diagnosis is now treatable thanks to this drug.
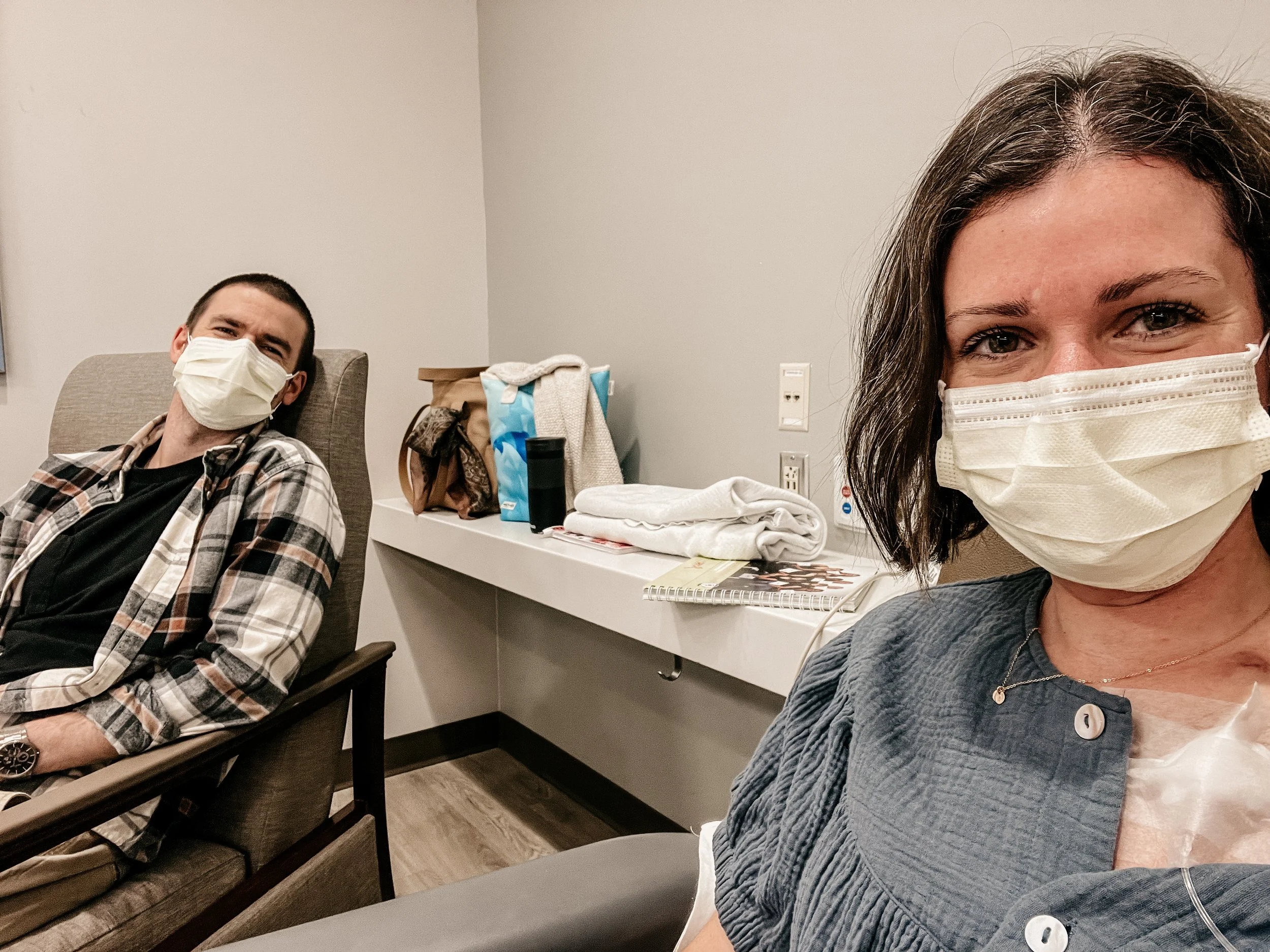
We arrived at the infusion center at 9am. They accessed my port and drew blood for labs to get a baseline before I start treatment. While we waited for labs, my nurse navigator that works with my oncologist came to educate us regarding treatment. The side effects she listed were ones I’ve read online and talked about with others - fatigue, nausea and other GI issues, low blood cell counts/weakened immune system, low platelets, pain in the joints and muscles, mouth sores, etc. The most common side effects are neuropathy in fingers and toes, and of course, hair loss. In the couple days after chemo treatment my bodily fluids are considered toxic (cue Brittany Spears)… with having little ones at home the nurse wants us to take extra precautions so they don’t have exposure to the chemo drug that may effect their future fertility or risk of other cancers (scary!). Using separate toilets, no lip kisses/sharing drinks, washing clothes separately, washing off sweat, etc. It might be extreme precautions but ones we’re willing to do. It was hard for E to understand yesterday, but we explained that I’m getting treatment for cancer that only I need, and the rest of the family doesn’t need this treatment, it comes out of my body through these ways so for only a couple of days we need to do these silly things!
I signed a consent for treatment and it listed the reason for treatment, checked off by my oncologist was CURE OF CANCER (vs. slow cancer growth, etc). I knew this was our goal after speaking with my medical team at the beginning, but seeing it in writing on that form felt amazing and reassuring!
We started treatment with Herceptin first. They do the first one slower for 90 minutes, the remaining treatments of Herceptin will faster at 30 minutes since I tolerated it well. Then they gave me premeds before Taxol - benedryl, steroid, anti-nausea. The benedryl made me tired so I was trying to take a nap as Taxol started.
The other possible side effect to Taxol is a hypersensitivity reaction, typically to the vehicle/compond of the drug…. and within 5 minutes of starting I woke up and knew something was wrong. My face was flush and hot, and my throat and chest started to tighten. I looked at Casey and told him something’s wrong, and I immediately hit the call button for a nurse. An RN was near my area and took one look at my face and knew I was having a reaction. She stopped the infusion and I started to feel immediate relief. Within seconds my nurse, other nurses and RNs, the pharmacist, and the on floor oncologist were there and giving me more steroids and other meds. I felt better, but the experience was terrifying and my body was shaking. We waited 30 minutes and rechallenged the Taxol, starting it again at 25% infusion rate. If I reacted again, we would have to meet with my oncologist to come up with a new treatment plan. It felt discouraging and I prayed that I could get through the rechallenge. Thankfully I tolerated 25% rate well and hung out there for about 2 hours. We slowly began increasing every 15 minutes and got up to 75% infusion rate, and then I was done with my first treatment! The original infusion rate would be 1 hour of Taxol infusion, but mine took about 4 hours.
The infusion staff at IU Schwarz Cancer Center was amazing, their knowledge, experience, and kindness got me through that first treatment. My nurse sat next to me during the entire length of the rechallenge, the on floor oncologist and pharmacist stayed with us until my infusion was done at close to 6pm. It was a LONG day, but #1 of 12 is DONE! Ellie made a chain with 12 paper links, and we tore one off when I got home… then of course had a dance party to celebrate!
The steroids are still working well, I feel like I could conquer the world today. I also feel like a ticking time bomb though, waiting to see what side effects I have in the next few days. Trying to keep a positive mindset and reminding myself that I can handle it! (I’m convinced moms have super powers…)
Current mantras:
I accept my circumstances as they unfold and trust in the ability of my body and medical team to overcome whatever is presented to me.
I release my feelings of fear and anxiety about cancer treatments. My feelings are messengers and I am the leader.